Healthcare law and regulatory consultant discusses the One Big Beautiful Bill Act’s new §71113 that prohibits federal direct spending Medicaid payments to prohibited entities that provide abortion services.
The recently enacted One Big Beautiful Bill Act (OBBBA)’s §71113, effective July 4, 2025, imposes a one-year prohibition on federal direct spending payments for Medicaid-funded abortion services by prohibited entities. Although Planned Parenthood Federation of America, Inc. (PPFA) may be the predominant provider of Medicaid-funded abortion services that is intended to be included in the definition of prohibited entities, hospital systems or non-profit arms of those systems, individual inpatient or rural hospitals, and rural health clinics that provide abortions may also be deemed prohibited entities subject to losing Medicaid funding.
Prohibited Entities
Section 71113 covers entities that are funded by state Medicaid agencies and Medicaid managed care organizations contracted with state Medicaid agencies, including managed care organizations, prepaid inpatient health plans, and prepaid ambulatory health plans.
Prohibited entities (and their affiliates, subsidiaries, successors, and clinics) covered by the law include those that met a combined federal and state matched Medicaid funding threshold that exceeded $800,000 across any one entity’s affiliate system in federal fiscal year 2023, and
are:
- exempt from taxation by being described in §501(c)(3) of the Internal Revenue Code (the “Code”); and
- primarily engaged in family planning services, reproductive health, and related medical care; and
- essential community providers as defined in 45 C.F.R. §156.235 (including family planning providers; inpatient hospitals; rural emergency hospitals; rural health clinics; and sexually transmitted disease clinics); and
- providers of “elective abortions” that exceed the scope of the Hyde Amendment criteria (the pregnancy is the result of rape or incest or there is a life-endangering physical condition caused by or arising from the pregnancy that would, as certified by a physician, place the woman in danger of death unless an abortion is performed).
As with any law, the executive and judicial branches of government can be left with ambiguous language that poses challenges to interpreting applicability. In §71113(b)(A)(ii), “primarily engaged” is not defined with any floor for the services of interest. Does “primarily” equate to 51% of claims? 75% of claims? 90% of claims? Furthermore, prohibited entities can be “primarily engaged” in any of the following services – not just abortion services: “family planning services, reproductive health, and related medical care.” Both “related medical care” and “reproductive health” are broad in scope and therefore also pose challenges to interpreting applicability of the law. In 2024, US HHS amended the Healthcare Portability and Accountability Act of 1996 (HIPAA) Privacy Rule via Final Rule and amended the definition of “reproductive health” to "…means health care, as defined in this section, that affects the health of an individual in all matters relating to the reproductive system and to its functions and processes. This definition shall not be construed to set forth a standard of care for or regulate what constitutes clinically appropriate reproductive health care.” 45 C.F.R. Section 160.103.
Beyond PPFA:Non-Profit Hospitals and Rural Clinics
The essential community providers that would expect to meet the requisite description and factors of a prohibited entity are family planning providers such as Planned Parenthood clinics. In fact, in early July 2025, PPFA, Inc., Planned Parenthood League of Massachusetts, and Planned Parenthood Association of Utah sued the US Department of Health and Human Services (HHS) and the Centers for Medicare and Medicaid Services (CMS), which regulates the Medicaid program, because, as they laid out in their Complaint:
“There is no legitimate justification for the statute; rather, the true design of the Defund Provision is simply to express disapproval of, attack, and punish Planned Parenthood, which plays a particularly prominent role in the public debate over abortion and (if Planned Parenthood’s Members are treated collectively) is the only nationwide abortion provider.” (D. Mass.), Case No. 1:25-cv-11913, Complaint for Declaratory Judgment and Injunctive Relief, p., ¶ 10.
Prohibited entities may also include hospital systems or non-profit arms of those systems, individual inpatient or rural hospitals, and rural health clinics that provide “elective abortions.” On July 7, as a result of the PPFA lawsuit, a federal district judge stayed implementation of §71113 for 14 days with a Temporary Restraining Order (TRO). The stay was not limited to the application of the law to Planned Parenthood clinics. On July 21, a federal district judge issued an Order for a preliminary injunction specific to the Plaintiffs in the case versus all potential prohibited entities. The Order prohibits the US HHS and CMS "…from enforcing, retroactively enforcing, or otherwise applying the provisions of §71113…against Planned Parenthood Association of Utah and other Planned Parenthood Federation of America Members who will not provide abortion services as of October 1, 2025 [the implementation date set forth in §71113(b)(1)(A)], or for which the total amount of Federal and State expenditures under the Medicaid program under title XIX of the Social Security Act for medical assistance furnished in fiscal year 2023 made directly to them did not exceed $800,000.” The preliminary injunction therefore does not prohibit implementation of the §71113 prohibition of federal direct spending Medicaid payments to prohibited entities that provide abortion services.
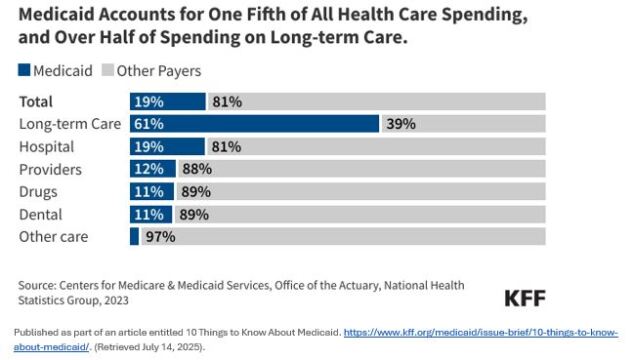
The Kaiser Family Foundation (KFF) published the following analysis of national Medicaid spending in comparison to other Health Care spending nationwide in 2023. On average, the Medicaid spend on hospital services comprised 19% of hospital revenue. However, hospital care accounted for about one-third (32%) of Medicaid spending in 2023.
Under the new law, 501(c)(3) hospitals that render abortion services which exceed the scope of the Hyde Amendment could subsequently lose federal Medicaid funding and struggle to maintain operations.
Keep in mind that prohibited entities will not include those entities that, along with all of their associated entities, strictly receive Medicaid reimbursement for abortion services that fall within the Hyde Amendment exceptions. Speaking of exceptions, you may find exceptions to the general rule by state.
State Abortion Laws and State-Specific Medicaid Coverage Policies
Although federal case law, statutes, and regulations control, more restrictive State abortion laws and State-specific Medicaid coverage policies may completely prohibit Medicaid reimbursement for any abortion procedures.
In 2022 when the Supreme Court of the US overturned Roe v. Wade, it returned abortion law discretion to the states. As a result, some states ban all abortions–including Medicaid-funded abortions–while other states have a continuum of gestational limitations and abortion ban exemptions for some or all of the Hyde Amendment elements. For example, in the southeastern US, the contiguous states of Virginia, North Carolina, South Carolina, and Tennessee have diverse state laws ranging from a total abortion ban in TN (except in cases of life or health of the mother) to legal abortions in North Carolina and South Carolina with exceptions that mirror the Hyde Amendment but with varying gestational limits. But note: South Carolina bars Planned Parenthood clinics from participating as Medicaid providers. For a summary of Medicaid-funded abortion coverage by state, see Kaiser Foundation, State Funding of Abortions Under Medicaid (Nov. 6, 2024).
States in which abortion is legal and in which abortion is a Medicaid-covered service have different clinical coverage definitions and qualifying criteria for Medicaid beneficiaries.
The statutory analysis of new §71113 does not specifically exempt the aforementioned Hyde Amendment. The section specifically excepts entities from being covered by the statute if the “elective abortions” are based on specific language that mirrors the Hyde Amendment. Medicaid is a federal-state funded entitlement program regulated by CMS, Medicaid state plans and waivers, state laws and regulations, and state Medicaid program and managed care plan clinical policies. Beyond the state law disparities noted above, individual state Medicaid program terminology for legal, covered abortions within the scope of the Hyde Amendment may differ further.
Comparison of North Carolina and Kansas as an example of differing Medicaid reimbursement and §71113 treatment of elective abortions.
Take for example, a comparison of North Carolina Medicaid and the Kansas Medicaid administrator, KMAP. North Carolina Medicaid uses the terms “therapeutic” and “non-therapeutic” abortion to establish when procedures will be reimbursed under the Medicaid program. North Carolina Medicaid defines therapeutic abortions as being, “the termination of a pregnancy where fetal heart tones are present at the time of the abortive procedure…" and expands on this definition with "[t]his includes the delivery of a non-viable (incapable of living outside the uterus) but live fetus, if labor was augmented by Pitocin drip, laminaria suppository, etc.” North Carolina Medicaid Clinical Coverage Policy No: 1E-2 (Feb. 15, 2024). As a general rule, North Carolina law prohibits abortion after the first 12 weeks of pregnancy (NC Gen. Stat. §90‑21.81A). However, North Carolina law also provides that, "...it shall not be unlawful to procure or cause a miscarriage or an abortion in the State of North Carolina in the following circumstances…[d]uring the first 24 weeks of a woman’s pregnancy, if a qualified physician determines there exists a life‑limiting anomaly…" NC Gen. Stat. §90‑21.81B. This interpretation of the Hyde Amendment in North Carolina’s laws could yield Medicaid reimbursement for an abortion procedure that was not included in the procedures excepted in §71113. Furthermore, NC Gen. Stat. §90‑21.81B requires the procedure to be performed by, "…a qualified physician licensed to practice medicine in this State in a hospital, ambulatory surgical center, or clinic certified by the Department of Health and Human Services to be a suitable facility for the performance of abortions…".
KMAP uses the term “elective abortion.” In Kansas, KMAP limits reimbursement to the statutory definition excepted from “elective abortions” and defines those in the Kansas statutes as, “an abortion for any reason other than to prevent the death of the mother upon whom the abortion is performed…" K.S.A. 65-4a01. The Kansas rules would prohibit all Medicaid reimbursements not covered by the portion of §71113 that tracks with the language of the Hyde Amendment as opposed to how North Carolina could potentially include a broader scope of Medicaid reimbursement circumstances.
Emergency Medical Treatment and Labor Act
Hospitals must also navigate §71113 in tandem with the application of EMTALA.
A potentially legally challenging scenario for hospitals is when a woman who is experiencing a health emergency that arises from a pregnancy comes to an emergency department. Regardless of whether the pregnancy was a result of rape or incest, and regardless of state abortion laws, including abortion bans, hospitals have been required to treat and stabilize women under the Emergency Medical Treatment And Labor Act(EMTALA). That treatment might include an abortion. However, on May 29, 2025, CMS rescinded existing, abortion-specific guidance on the implementation of EMTALA. Then on June 24, Attorneys General from 21 states including NC wrote to the American Hospital Association with the message, “CMS’ rescission of this regulatory guidance does not change federal law or the obligations EMTALA imposes. Put simply, all hospitals must continue to follow EMTALA, including with respect to the provision of emergency abortion care. We therefore ask that you remind your members of their continuing obligations under EMTALA.” The legal implications for 501(c)(3) hospitals remain to be seen, but EMTALA treatment that included abortion procedures in FFY2023 could potentially qualify these hospitals as prohibited entities that are ineligible for Medicaid funding.
Takeaways for Organizations that May Be Covered by §71113
The potential for the new §71113 to cover provider entities other than family planning clinics structured similarly or the same as PPFA and associated entities should not be overlooked by hospitals and other essential community providers that are also exempt from taxation by being described in 501(c)(3) of the Code. A potential approach to determining applicability might include:
1. Identify all entities that are affiliated with the potentially covered entity, as described in §71113; and
2. Determine whether the total value of Title XIX federal and state medical assistance to the entity and its affiliate exceeded $800,000 for the 2023 federal fiscal year; and
3. Determine whether the potentially covered entity is an essential community provider as described in §156.235 of title 45 of the Code of Federal Regulations; and
4. Determine whether the entity is primarily engaged in family planning services, reproductive health, and related medical care and provided any abortion services not specifically exempted by §71113(b)(1)(A)(iii).
If each of the above factors applies, regardless of whether the organization considers itself a family planning provider, then the entity is likely to qualify as a prohibited entity ineligible for all federal Medicaid payments under the new law.
One possible way to avoid being a qualified prohibited entity under §71113 is for Medicaid providers to voluntarily forfeit their 501(c)(3) status. However, agencies may want to conduct comprehensive “return on investment” analyses to weigh the potential for income tax savings against the loss of 501(c)(3) status eligibility for current and future federal, state, and local grants, cooperative agreements, and foundation funding. In addition to Medicaid reimbursement, these funding streams are often integral to agencies’ operational sustainability.
As of the date of publication of this article, the PPFA lawsuit is still pending. Additional legal challenges to the application of §71113 may arise in courts as more healthcare entities determine that they qualify as prohibited entities under the law.
This article does not necessarily reflect the opinion of Bloomberg Industry Group, Inc., the publisher of Bloomberg Law, Bloomberg Tax, and Bloomberg Government, or its owners.
Author Information
Sarah Pfau, JD, MPH is a healthcare law attorney and a 30-year career public health professional with expertise in Medicaid program CMS, State government, health plan, and provider agency operations at Sarah E. Pfau, Attorney at Law, PLLC.
Write for us: Author Guidelines
To contact the editor responsible for this story: Soni Manickam at smanickam@bloombergindustry.com
Learn more about Bloomberg Tax or Log In to keep reading:
See Breaking News in Context
From research to software to news, find what you need to stay ahead.
Already a subscriber?
Log in to keep reading or access research tools and resources.